
Proactive Healthcare Interoperability Dashboard
Smart Interface Observability for Every Hospital
Executive Brief At 2:47 a.m., one HL7 channel failure between your EHR and laboratory system stops order processing. Results never post. By 7:00 a.m., two ER beds remain blocked, three discharges stall, and $12,000 in direct productivity loss is already incurred according to the Ponemon Institute's Cost of Data Center Outages 2022 (scaled per bed count for small facilities).
For leaders of community health centers, Critical access hospitals and rural hospitals, this scenario represents the predictable result of reactive integration management. The financial, clinical, and regulatory consequences are now quantifiable, material, and rising.
The Strategic Imperative of Interoperability
For hospital executives and CIOs, interoperability has evolved from a technical detail to the core driver of revenue integrity, regulatory compliance, and clinical throughput.
In a 25 bed facility, one integration failure ripples through the revenue cycle:
- Laboratory orders require manual re entry, delaying results by four to six hours.
- Payer eligibility checks time out, driving 15 to 20 percent claim denials at $118 average rework cost as detailed in the CAQH 2023 CAQH Index Report.
- Imaging results stay siloed, leading to 10 to 30 percent duplicate diagnostics at $1,000 to $5,000 per test.
Each unmonitored interface compounds these inefficiencies. The result: hundreds of hours in staff rework and hundreds of thousands of dollars in preventable annual losses often 3–5 % of net patient revenue for small and mid-sized hospitals.
The scale is national. Integration inefficiencies drive an estimated $30 billion in avoidable healthcare spend annually (CAQH Index 2023; Healthcare IT News 2024).
Yet, despite massive investment in EHRs, only 43% of U.S. hospitals routinely exchange and integrate patient data across all interoperability domains (ONC Interoperability Data Brief 2023).
The gap isn’t about technology it’s about visibility. Without real-time integration health metrics, hospital leaders manage reactively, discovering failures only after they disrupt care or revenue. In a compliance-driven landscape, that’s no longer sustainable.
The Root Causes of Reactive Integration
Why do so many healthcare organizations still struggle to manage integrations proactively?
For rural and community hospitals, the barriers are both structural and human, a mix of constrained budgets, limited expertise, and vendor dependencies that keep them trapped in reactive mode.
The obstacles are structural and profoundly human.
-
Chronic Underinvestment in IT
Most rural hospital IT budgets remain modest, typically under $500,000 annually (Chartis Rural Health Report 2024). Hiring even one integration engineer, with median compensation between $110,000 and $130,000 (Glassdoor Salary Data 2025), consumes nearly a quarter of available funding.
When you add monitoring tools, training, and 24/7 coverage, a full in-house integration team becomes financially out of reach.
-
Scarcity of Specialized Talent
Technical capability remains another limiting factor. Fewer than 15% of rural IT staff report formal HL7 or FHIR training, and turnover is high. When that one certified expert leaves, years of institutional knowledge disappear, leaving hospitals to rely on external consultants or reactive troubleshooting.
-
Vendor Limitations and Dependence
EHR vendors provide excellent clinical platforms, but custom integration management isn’t their core strength.
- athenahealth performs well within its marketplace, but connecting external labs or imaging centers often requires $50,000+ professional services.
- eClinicalWorks (eCW) offers HIE connectivity through eEHX, yet users report 3–6 month delays and 20–25% claim denials due to sync.
- Kareo/Tebra, designed primarily for billing, struggles with multi-system workflows and integration.
The result: hospitals depend on vendors for basic connectivity but shoulder full responsibility when integrations break.
Compliance Pressures: The Regulatory Squeeze on Small Hospitals
Imagine your next audit. An Office for Civil Rights (OCR) letter arrives. Or CMS identifies an ADT notification failure. In small hospitals, compliance is essential, not optional. Yet reactive integrations restrict your options.
Current regulations overlap and intensify. One integration failure can breach HIPAA, ONC, CMS, and FHIR standards simultaneously.
- HIPAA Security Rule requires continuous risk monitoring and audit ready logs for every ePHI flow. In 2025, over 540 breaches exposed 112 million records, with third party integrations as OCR’s top enforcement focus, fines up to $2.1 million per violation.
- ONC’s Cures Act prohibits information blocking and mandates FHIR APIs under §170.315(g)(10). Noncompliance risks $1 million per violation.
- CMS 9115 F mandates FHIR based ADT notifications and patient access APIs (USCDI v3 by 2026). Failure invites 5% Medicare payment cuts and MIPS penalties.
- FHIR serves as the new compliance language, but a “certified” endpoint offers no protection if the channel fails silently from queue backlogs or authentication drift.
Consider a lab result that never reaches the EHR:
- HIPAA: Breach of security safeguards.
- ONC: Information blocking.
- CMS: Missed ADT event.
- Total exposure: Over $3 million in fines and payment reductions.
Your small team cannot manually log every HL7 message or troubleshoot FHIR errors at 3 a.m. Unmonitored integrations attract audits, not just risks.
The Open-Source Integration Dilemma: When Flexibility Meets Risk
For years, open-source integration engines have powered interoperability across hospitals and clinics. Tools like Mirth Connect, NextGen’s open-source predecessor, and other community-maintained frameworks offered a cost-effective way to connect EHRs, labs, payers, and imaging systems without vendor lock-in.
But the ground has shifted. What was once a strategic advantage is now a compliance and security liability.
The reality: most open-source engines no longer provide enterprise-grade safeguards—no vendor patches, no Business Associate Agreements (BAAs), and no guaranteed security updates. This exposes hospitals to unmonitored vulnerabilities and potential HIPAA violations.
-
Case in point – Mirth Connect:
On March 19, 2025, NextGen Healthcare transitioned Mirth Connect to a closed-source model (v4.6+). Older open-source versions (≤4.5.2) are now static—no official updates, no vendor accountability, and no compliance coverage.
Known exploits such as CVE-2023-43208 (remote code execution) remain unpatched. While community forks like BridgeLink attempt to fill the gap, they lack regulatory validation and long-term support assurances.
For hundreds of small hospitals on legacy Mirth, this is not an upgrade; it is a compliance precipice.
The risks are immediate and profound:
- Compliance: Full liability across HIPAA, ONC, and CMS, $50,000 to $2.1 million plus in fines and audits.
- Downtime: Silent channel failures cost $7,900 per minute; one incident can surpass $740,000.
- Data Breaches: Unpatched code invites attacks, average cost $9.77 million.
Operating unmanaged open source Mirth is no longer economical.
Community forks like BridgeLink provide continuity, but regulatory support not there yet.
Open-source integration isn’t inherently bad, but running it without managed observability, patching, or compliance controls is no longer viable.
The Smarter Path: Proactive Integration Management
Instead of waiting for failures, leading community hospitals are shifting to Managed Observability as a Service: a proactive model that fuses enterprise grade technology with 24/7 human expertise.
At KPi Tech, we deliver exactly that.
-
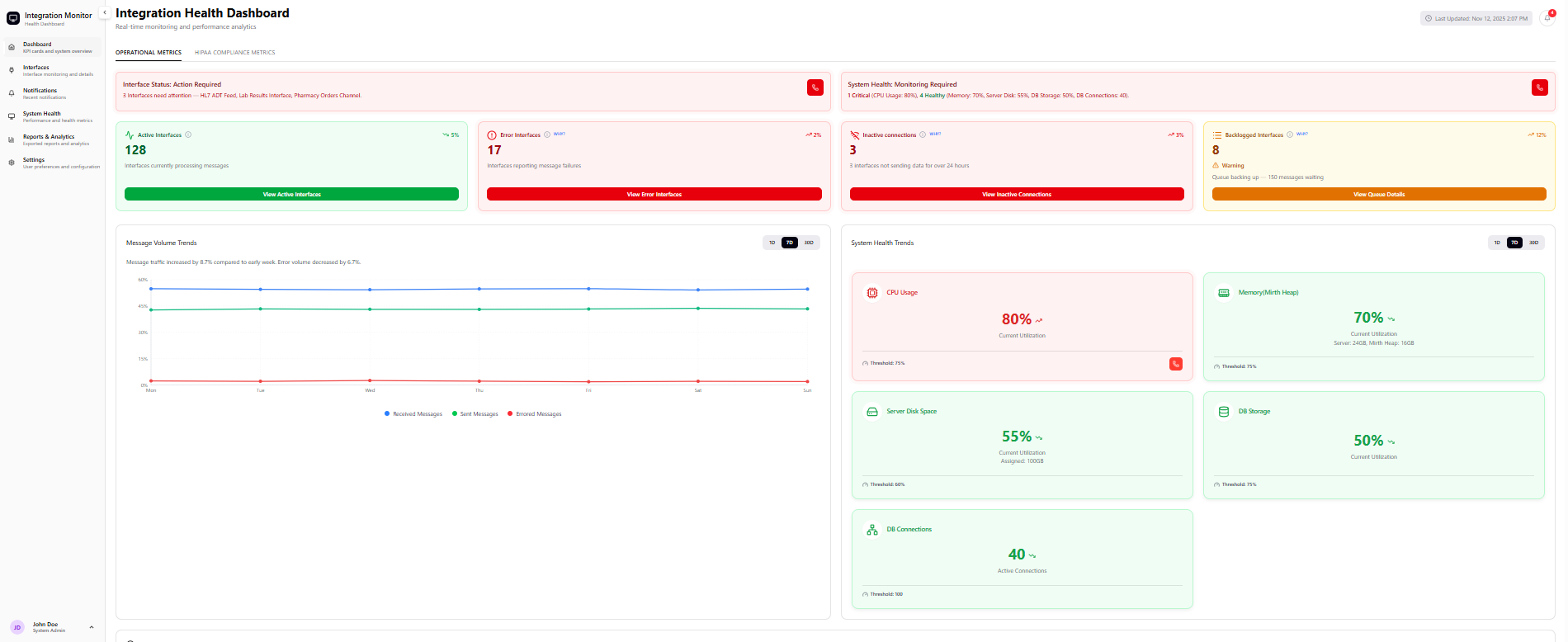
Managed Observability Dashboard
KPi does not merely monitor integrations; it orchestrates them. Our fully managed, HIPAA BAA platform integrates enterprise grade observability with 24/7 expert InterfaceOps, no additional headcount, infrastructure, or compliance gaps.
-
The Dashboard That Sees Everything
Powered by Datadog and hosted in a secure HIPAA BAA environment, KPi provides:
- Real time JMX telemetry: message volume, queue depth, error rates, latency.
- PHI scrubbed, immutable logs with predictive anomaly detection.
- Automated compliance reporting: uptime, SLAs, FHIR health, audit trails (PDF/CSV export).
- Zero maintenance: we host, scale, and update it.
-
Your Remote Integration Department
Our InterfaceOps team, HL7/FHIR certified engineers available 24/7, delivers:
- MTTR under two hours for critical incidents (P1) (contractually guaranteed).
- Full lifecycle management: design, validate, deploy, optimize.
- Direct Tier 2/3 support: no more “call your vendor.”
- Cross engine mastery: open source Mirth, NextGen Mirth, Rhapsody, Corepoint.
And KPi aligns automatically with HIPAA, ONC, CMS, and FHIR. No add ons. No custom scripts. Compliance is embedded.
ROI: From Risk to Resilience
The metrics are compelling:
| Metric | Reactive Baseline | KPi Enabled | Annual Impact (25 Bed Facility) |
|---|---|---|---|
| Uptime | 95 to 97 percent | >99.9 percent | $190,000 to $720,000 saved |
| Claim Denials | 15 to 20 percent | ↓ 21% | $40,000 to $120,000 recovered |
| Duplicate Testing | 10 to 30 percent | ↓ 25% | $24,000 to $96,000 saved |
| Staff Time | One to two hours/day lost | Reclaimed | 480 to 960 clinical hours/year |
| Audit Prep | 40+ hours/audit | ↓ 40% | 16 to 20 hours saved |
Total Cost of Ownership
- In House Build: $250,000+ (two FTEs plus tools plus on call).
- KPi Managed Service: (Dashboard + 24/7 InterfaceOps + compliance + updates + support) : $36,000 to $60,000.
- Your Savings: Approximately 76 percent ($190,000+).
See how KPi-Tech helps hospitals move from interface failures to ROI gains.
Sustained Success: Beyond Go Live
KPi is a partnership, not a project. We track:
- Integration uptime (>99.9 percent).
- Error rate per 1,000 messages.
- MTTR, denial trends, staff time saved.
You receive monthly compliance ready reports and quarterly roadmap reviews, ensuring you anticipate ONC, CMS, and OCR changes.
Conclusion: Your Move to Proactive
Small hospitals face enterprise grade mandates with community resources.
The Open Source engine licensing shift, EHR integration blind spots, and multi agency regulatory pressures have created a perfect storm.
KPi Managed Observability as a Service is your lifeline:
- Compliance grade visibility across HIPAA, ONC, CMS, and FHIR.
- 24/7 expert InterfaceOps: your remote integration team.
- 76 percent lower cost than in house.
Our InterfaceOps team can monitor, patch, and support your interfaces remotely, whether on legacy Mirth, athenahealth, eClinicalWork, Kareo, or any combination.
Stop reacting. Start preventing.
Next Step: Let us help you to map your Mirth exposure, EHR gaps, and deliver a customized ROI projection within 48 hours.
Schedule a free 30 minute risk assessment.Savings estimates based on peer outcomes and industry benchmarks. Actual results vary.




