
How can EHRs like Epic, Cerner, and MEDITECH be Integrated Cost Effectively
Electronic Health Records EHR adoption rates have significantly increased, reaching an impressive 96%. Both small and large healthcare providers are now embracing EHR systems like Cerner, Epic, and MEDITECH to manage patient information electronically. These EHR systems serve as a foundation, allowing healthcare organizations to add additional applications on top, creating a comprehensive solution that connects healthcare data and ensures controlled access.
While the benefits of EHR integration are evident, it also presents challenges in terms of interoperability. Implementing EHR integration requires expertise in API integration and familiarity with interoperability standards, which many healthcare companies lack. As a result, these organizations often seek assistance from tech partners to help them integrate various third-party solutions with their EHR or EMR platform.
Epic EHR System:
Epic Systems Corporation is an EHR company based in Verona, Wisconsin, founded in 1979. As of 2021, Epic holds a 31% market share in the EHR industry.Its primary focus is on large healthcare organizations and hospital systems, with clients including Cleveland Clinic, Johns Hopkins, and Mayo Clinic.
Key Features:
- MyChart: Patient portal allowing appointment scheduling, access to medical records, and medication refill requests.
- EpicCare: Main portal with versions for ambulatory and inpatient settings.
- Care Everywhere and Share Everywhere: Platforms for sharing medical records between organizations and between patients and clinicians.
- Healthy Planet: A module for analyzing patient populations and identifying care gaps.
Strengths:
- Strong user interface: Praised for its intuitive design and workflow efficiency, with high customization options.
- Focus on interoperability: Dedicated platforms like Care Everywhere and Share Everywhere enable data sharing between organizations using Epic EHR.
- Improved patient engagement: MyChart patient portal facilitates patient involvement in treatment, appointment scheduling, and communication with healthcare providers.
Weaknesses:
- High cost and complexity: Epic is the most expensive EHR system, requiring extensive investment in software, hardware, implementation, training, and maintenance.
- Lack of extensive integration with non-Epic systems: Limited integration with other systems due to proprietary architecture and data sharing concerns
EPIC Implementation Cost
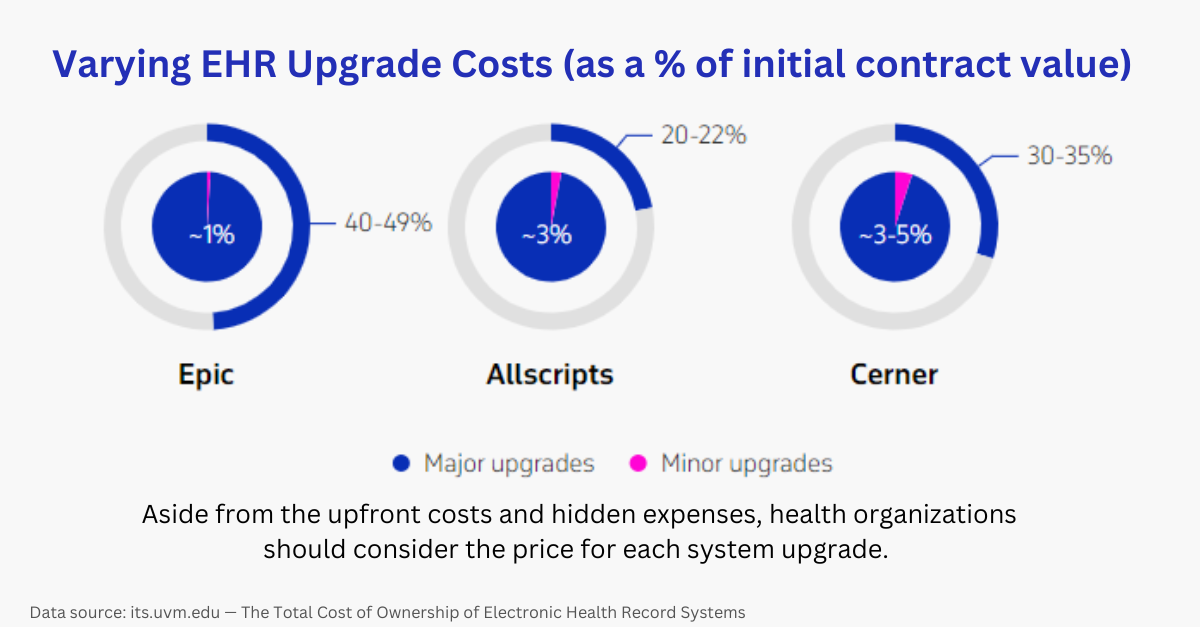
Epic's pricing structure varies depending on the size of the client company and the number of system users. Unfortunately, Epic does not provide a trial version or a clear breakdown of costs. According to Forbes' investigation, self-hosted solutions start at $1,200, while clinics and hospitals may have an average cost of around $500,000. Training fees are approximately $2,000 per organization, and additional expenses can range from $200 to $35,000 per month.
Best Practices for Integration:
- Develop a data mapping and migration strategy for a smooth transition to Epic EHR.
- Utilize Epic's interoperability capabilities as needed for the organization.
- Consider customization options that align with specific workflow requirements.
- Allocate ample time for staff training due to the system's complexity.
- Ensure a dedicated IT team to navigate the integration process.
Cerner EHR system
Cerner Corporation, founded in 1979 and headquartered in Kansas City, Missouri, is a major provider of health information technology services.
Cerner holds the second-largest market share in the EHR industry, standing at 25% as of 2020. With a global presence, the company operates in 35 countries, serving hospitals and healthcare systems of all sizes. Notable clients include the U.S. Department of Defense and the U.S. Department of Veterans Affairs.
Key Features:
- Cerner PowerChart Ambulatory: Designed for physicians in various practice sizes, offering E-prescribing, chart search, patient portal, and more.
- HealtheIntent: A population health management platform focused on data aggregation and care coordination for different populations.
- Cerner Millennium: The company's flagship product for large hospitals, providing documentation, data analysis, reporting, and drug alerts.
- CareTracker by Cerner: A dedicated platform catering to care centers and assisted living facilities.
- CareTracker by Cerner: A dedicated platform catering to care centers and assisted living facilities.
- HealtheLife: Cerner's patient platform enabling patients to access their health information.
Strengths:
- Scalability: Cerner's EHR system is highly scalable and adaptable for both large and small healthcare organizations, thanks to its modular architecture, allowing flexible implementation of different modules.
- Extensive Experience: With over 40 years in the market, Cerner has gained experience across various healthcare settings, making it well-suited for different healthcare structures.
- Interoperability: Cerner surpasses Epic in interoperability by not only integrating with its own systems but also extending support to competitors through an open integration API policy. It supports various interoperability standards like HL7, FHIR, and CDA, enhancing data exchange capabilities.
Weaknesses:
- Non-Intuitive User Interface: Some nursing professionals find Cerner's interface less intuitive compared to Epic, with difficulties in finding certain functions and managing multiple windows simultaneously.
- Complex Implementation and Customization: While less complex than Epic, Cerner's software still requires comprehensive staff training. The options for customization are limited, making it challenging to tailor workflows for specific departments or individuals.
Cerner Implementation Cost
Cerner is the most popular EHR platform provider for individual practitioners, as they offer an annual subscription plan for their basic cloud-based solution for $25 a month. However, they have around 50 speciality-focused products and on-premise systems that are much more expensive.
Best Practices for Cerner EHR Integration:
- Carefully select relevant customization options and modules for your organization.
- Provide extensive training for staff members involved in using the Cerner system.
- Leverage interoperability with Cerner's native systems and other third-party applications.
- Prioritize data cleansing, migration, and validation during the migration process.
Meditech EHR System
MEDITECH, also known as Medical Information Technology, Inc., is a Massachusetts-based company that provides EHR systems to healthcare organizations worldwide. Established in 1969, it holds a 16% market share and focuses on serving smaller hospitals and community healthcare facilities.
Key Features:
- MEDITECH Expanse: A web-based EHR portal offering billing, e-prescriptions, scheduling, and access to patient information for clinicians.
- MEDITECH Surveillance: Real-time analysis of patient healthcare information.
- MEDITECH Patient Portal: A tool for patients to manage their information and appointments.
Strengths:
- Cost-effectiveness: Compared to Epic and Cerner, MEDITECH is more affordable due to its simplified features and transparent pricing model without hidden costs.
- Ease of Implementation: Tailored for smaller healthcare organizations, MEDITECH offers a straightforward implementation process with standard training modules.
- Population Health Management: MEDITECH provides robust tools for tracking individual patient health outcomes and care coordination, supporting population health management.
Weaknesses:
- Limited Third-party Integration: MEDITECH's integration capabilities are weaker compared to Epic and Cerner due to its use of a proprietary system and reliance on the HL7 protocol only.
- Weak User Interface: The MEDITECH interface is less developed and less intuitive than Epic and Cerner, partially due to budget constraints. Efforts to improve the interface are ongoing with features like Expanse.
Best Practices for MEDITECH EHR Integration:
- Follow MEDITECH's standardized implementation process and utilize available resources.
- Involve all stakeholders early on in the implementation to ensure the system meets everyone's needs.
- Clearly outline specific organizational goals before starting the implementation process.
RELATED: EHR Integration Guide
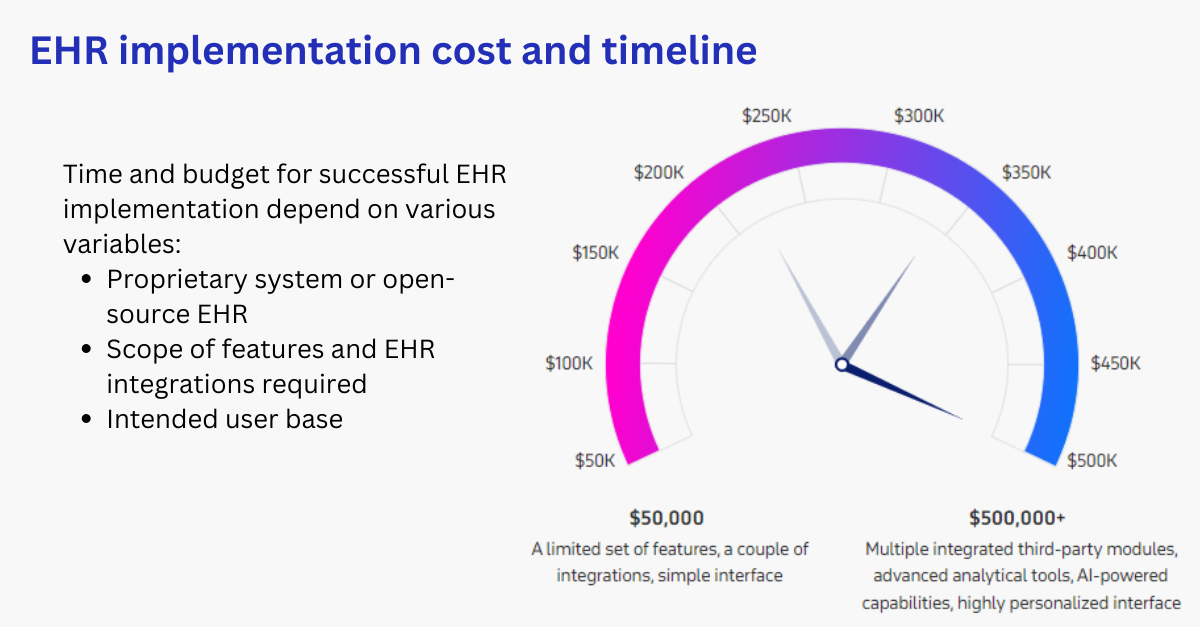
EHR Implementation cost
According to a Health Affairs study, a typical multi-physician practice can anticipate spending approximately $162,000 for EHR implementation, with $85,000 allocated to first-year maintenance expenses. Though these estimates are based on earlier EHR adoption stages, they still offer a useful reference for budgeting purposes.
Practices adopting an EHR solution can expect to recoup their investment in around two and a half years, enjoying an average net benefit of about $23,000 per year for each full-time employee thereafter.
Types of EHR Costs
-
Direct Expenses
-
Hardware Upgrades:Implementing an EHR system may require upgrading the organization's hardware infrastructure to meet the system's technical requirements. This could involve purchasing new servers, workstations, networking equipment, and other hardware components.
- Software License or Subscription:EHR vendors typically charge licensing fees for using their software. The cost can vary based on the number of users and the functionalities required. Alternatively, cloud-based EHR solutions often have subscription-based pricing models, where organizations pay a regular fee based on usage and features.
- Implementation Costs:The implementation phase involves configuring and customizing the EHR system to align with the organization's workflows and requirements. It may also include data migration from legacy systems to the new EHR platform. Implementation costs encompass expenses related to project management, consulting, and technical services provided by the vendor or third-party consultants.
- Hidden Costs:These are the additional, unforeseen expenses that may arise during or after the implementation process. Examples include costs associated with resolving unexpected technical issues, software updates, or additional customization requests not accounted for in the initial budget.
-
Hardware Upgrades:Implementing an EHR system may require upgrading the organization's hardware infrastructure to meet the system's technical requirements. This could involve purchasing new servers, workstations, networking equipment, and other hardware components.
-
Customization Costs
- Expenses Related to Tailoring the System:Customizing an EHR system involves adapting it to the specific needs and preferences of the healthcare organization. This customization can range from simple configuration changes to more complex modifications that require software development.
- Costs Associated with Network Updates:Integrating the EHR system with the existing network infrastructure may necessitate updates or enhancements to ensure smooth data exchange and system interoperability. Network updates may involve hardware, software, or security enhancements.
- Fees for Data Migration: Migrating patient data from legacy systems to the new EHR platform can incur costs. Data migration may involve data cleansing, validation, and mapping to ensure data accuracy and consistency in the new system.
- Unanticipated Expenditures:During the customization process, unexpected challenges or requirements may arise, leading to additional expenses. These unforeseen costs can include changes in regulatory compliance, user feedback, or modifications based on newly identified organizational needs.
-
Additional Costs
- Extra Storage Expenses:As healthcare organizations accumulate more patient data, they may need to allocate additional storage space to accommodate the growing data volumes. Additional storage can result in increased infrastructure costs or cloud storage fees.
- Initial Productivity Reduction:During the initial implementation phase, there may be a temporary reduction in productivity as staff members adapt to the new system. This can lead to operational inefficiencies and decreased patient throughput.
- Losses Due to System Downtime:System downtime can occur during upgrades, maintenance, or technical issues. These disruptions can lead to operational losses, reduced patient care efficiency, and potential revenue loss.
- Costs Related to Staff:The implementation of an EHR system may require additional training for existing staff or hiring new personnel with expertise in managing the system.
-
Staff Costs
- Training Costs for Personnel: Training staff members to effectively use the new EHR system is crucial for successful implementation. Training costs can include instructor fees, training materials, and staff time spent in training sessions.
- Expenses for Hiring New Staff:Depending on the organization's size and complexity, hiring new staff, such as EHR specialists or support personnel, may be necessary to manage and maintain the system effectively.
- Overtime Payments: During the implementation phase, staff members may need to work overtime to meet project deadlines, leading to additional labor costs.
It's essential for healthcare organizations to carefully plan and budget for these expenses during the EHR integration process to ensure a successful and cost-effective implementation.
RELATED: How EHR Optimization can Maximize ROI
Ways to reduce EHR implementation costs
- Consider Open-Source EHR:Installing an open-source EHR system may offer basic features at a low cost or even for free. If you lack IT specialists, hiring a developer to implement the open-source solution could be more cost-effective than choosing a proprietary EHR.
- Opt for Necessary Features and Integrations:Conduct a thorough analysis of your organization's needs and prioritize essential functionalities. Avoid unnecessary "nice-to-have" features and non-vital integrations to cut down on costs.
- Choose a Subscription-Based Payment Model:Consider EHR systems with annual subscription payments to ease the upfront cost burden. This model offers flexibility to adapt the service plan as needed.
- Prioritize Data Security:Don't compromise on data security. Investing in a reliable, secure EHR system is crucial to prevent costly data breaches that are prevalent in the healthcare industry.
- Partner with Experienced EHR Developers:Collaborate with software companies with a track record of successful EHR implementations. Experienced teams can optimize costs and expedite the implementation cycle, allowing you to start benefiting from the system sooner.
How Healthcare Integration expert can Help lower EHR Integration and Implementation Cost
Healthcare integration experts play a crucial role in helping lower the cost of EHR implementation and integration by utilizing their specialized knowledge and experience. Here's how they contribute to cost reduction:
-
Efficient Planning and Strategy:
- Integration experts work closely with healthcare organizations to understand their specific needs and objectives.
- They devise a comprehensive integration plan and strategy that focuses on optimizing resources and minimizing unnecessary expenses.
- By identifying key requirements and potential challenges early in the process, they can prevent costly delays and setbacks.
-
Selecting Cost-Effective Solutions:
- Integration experts have in-depth knowledge of various EHR systems and integration tools available in the market.
- They can help healthcare organizations choose the most cost-effective EHR solution that aligns with their needs and budget.
- By avoiding overpriced or unnecessary features, they ensure that the organization invests in a system that provides maximum value for money.
-
Customization and Interoperability:
- Healthcare integration experts can customize the EHR system to match the organization's workflows and processes without overspending on extensive customizations.
- They focus on ensuring seamless interoperability with existing systems, which reduces the need for expensive integration efforts later on.
-
Data Migration Efficiency:
- Data migration is a critical aspect of EHR implementation and can be time-consuming and costly if not executed properly.
- Integration experts use their expertise to streamline the data migration process, ensuring data accuracy while minimizing downtime and potential data-related expenses.
-
Standardized Integration Protocols:
-
Reducing Downtime and Disruptions:
- Experienced integration experts carefully plan the implementation process to minimize system downtime and disruptions to healthcare operations.
- By efficiently coordinating the integration tasks, they can limit the impact on productivity and reduce potential revenue losses.
-
Compliance and Security:
- Healthcare integration experts ensure that the integrated EHR system complies with industry regulations and data security standards.
- By prioritizing data security, they mitigate the risk of costly data breaches and regulatory penalties.
-
Post-Implementation Support and Optimization:
- Integration experts provide ongoing support to address any issues that arise after the EHR implementation.
- They continuously monitor the system's performance and optimize it for better efficiency, leading to long-term cost savings.
In conclusion, healthcare integration experts bring a wealth of knowledge and experience to EHR implementation projects, enabling organizations to make informed decisions, minimize expenses, and achieve a successful integration that aligns with their budgetary constraints. Their expertise in planning, customization, data migration, and system optimization ensures that the EHR implementation delivers significant cost benefits and positively impacts overall healthcare operations.For cost-effective EHR integration and implementation, consider reaching out to KPi-Tech, a healthcare IT company with over 20 years of experience in providing healthcare IT services.





